By Cort Johnson
The Ron Tompkins Effect
Ron Tompkins had recently come back from a meeting with over a dozen MD’s and specialists from Mass General Hospital who’d evinced a strong interest in ME / CFS. Dr. Bateman has said it’s easy to get researchers, at least, interested in this disease but doctors – they tend to be the really tough sells. Yet, here was Tompkins, not long after creating the Harvard ME / CFS Collaboration with Wenzhong Xiao, PhD, meeting with 14 of them.

I wondered how that could have happened and then realized what was going on. It was the “Ron Davis effect” – showing up at Harvard. The effect occurs when a highly respected researcher takes ME / CFS on in a big way, causing the people around him to sign on. Ron Tompkins himself and the Center he leads is a result of the “Ron Davis effect”.
Tompkins has been at Mass General for 40 years, during which time he’s managed large research efforts garnering $200 million (gulp) in NIH grants.
Now the “Ron Tompkins effect” at Harvard – which has been funded by the Open Medicine Foundation – has produced a large team of international researchers and over dozen MD’s willing to collaborate on working on ME / CFS.
There’s more to it than that, though. Location does matter. Tompkins described Harvard and Mass General as hotbeds of medical and intellectual curiosity. The doctors there are used to dealing with complex cases of chronic illness. They tend to be heavily involved in research. They tend to thrive on challenges. They probably don’t succumb to dogma so easily.

Still, the idea that Tompkins was meeting with specialists – neurologists, rheumatologists, infectious disease specialists, and even a mitochondrial genetic specialist – was a shock to me. I thought Tompkins was leading an ME / CFS research center, but he is clearly thinking bigger than that.In fact, Tompkins reported that they call their ME / CFS patients their “five o’clock patients” because they tend to save them for the end of the day when they can spend more time with them. Sometimes, he reported, the doctor will be there long after the staff has gone home.
It turns out that Tompkins and Xiao want to transform how people with ME / CFS within the Harvard hospital system are treated as well. They want patients to get the right tests and get seen by the right specialists. They want the doctors they’re working with to be on the same page with regard to diagnostic protocols, standard testing protocols, referrals, etc. Ultimately, a kind of template could be created that groups at other institutions could use. The doctors’ group plans to meet quarterly.
Thinking Big – A Harvard Center of Excellence
It is the intent for the many clinicians and investigators at the Harvard-affiliated Hospitals to establish an institution-wide Center of Excellence for Chronic, Complex Diseases, THe Harvard ME / CFS Collaboration
As to the Center of Excellence? An academic medical center integrating medical and research efforts on the Harvard campus? That’s a major, long term goal but it’s one Tompkins is quite serious about.
The Center would not be just about ME / CFS – and that’s the good news. ME / CFS is clearly associated with diseases like fibromyalgia but has been sitting in its own little silo with its own researchers, conferences, and even doctors for decades – losing opportunity after opportunity for funding and understanding. It’s impossible that the quintessential pain and fatigue disorder (FM) couldn’t benefit from being studied with the quintessential fatigue and pain disorder (ME / CFS) but they rarely are. Since both suffer from similar funding issues, creating a center that focuses on them (and others) can only help everyone. That is what Tompkins aims to do.
By fostering collaboration between specialists who have long studied ME / CFS, post-treatment Lyme Disease, and Fibromyalgia in isolation, we aim to break down barriers and share learnings, leading to new advances in the understanding and treatment of these related diseases. Harvard Collaboration
The Center would draw on a wide variety of disciplines (internal medicine, primary care, infectious disease, neurology, surgery, neurosurgery, genetics, pediatrics, rheumatology, cardiology, pulmonology, psychiatry, psychology, and possibly others).
The really interesting thing about the potential Center is that the interest is already there. In fact, the interest in a potential Center has been so strong that Tompkins was convinced if he had the money, he could quickly open a fully staffed Center of Excellence on the Harvard campus. That’s pretty shocking. From the Collaborative Center website:
“The COE… would be extraordinarily well-supported by a very large group of extremely knowledgeable and committed clinicians and investigators at the Harvard-affiliated Hospitals as well as a key cohort of longstanding critical collaborators.”
“Complete implementation of a fully functional COE would be straightforward as there are dozens of clinicians and investigators who have been working independently for decades who would welcome the opportunity to work together as a very cohesive clinical and investigational internationally-recognized Center of Excellence.”
I don’t know about you but the sound of an internationally recognized Center of Excellence sends a shiver up my spine. Creating a Center like this would take a major philanthropic effort but because the Center would include ME / CFS, fibromyalgia, post-treatment Lyme disease and, I imagine, other neglected diseases (postural orthostatic tachycardia syndrome, Ehlers-Danlos Syndrome, mast cell activation syndrome, irritable bowel syndrome, Gulf War Illness, environmental illness, mitochondrial disorders), it’s got quite a large audience – and a very hungry audience – to draw from.

Put all those illnesses together and you have a patient population in the U.S. that runs to the tens of millions. None of these diseases or the people who have them are getting their due. Tens of millions of people are receiving substandard medical treatment and a mostly blind eye from the NIH. That’s tens of millions of people who would undoubtedly love to finally have a Center, at one of the top medical schools in the world, devoted to their illness.
That’s a pretty nice crowd to draw from. Anyone want to get their name on a building?
The Harvard Collaboration Takes on the Muscles and Exercise
Two studies are underway and many more are planned.
The Muscle Study
We all know about the exercise (activity) intolerance in ME / CFS – the disease is practically defined by it, but where is it coming from? Is it the immune system? The brain? The autonomic nervous system? The muscles? (All of them?)
It’s about time someone took a deep, deep, deep dive into the muscles in ME / CFS and that’s what the Harvard Collaboration is doing. Tompkins described an international effort stretching from the U.K. to Sweden to the U.S.
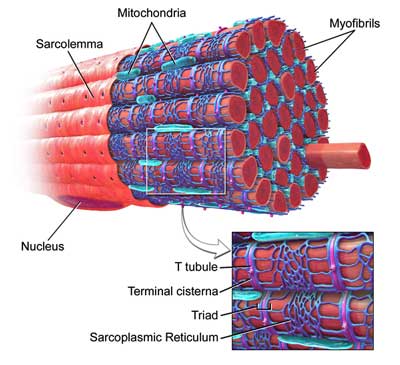
Their working hypothesis has a familiar theme – with a twist. They believe, like others, that exercise-induced inflammation (e.g. cytokines) is at the heart of the post-exertional malaise (PEM), but they’ve identified a different target. They believe exercise may doing lasting damage to the small myofibrills which make up our muscle fibers.
It’s true that exercise – or rather, “muscular stress” – damages myofibrills in healthy people (hence the aching muscles a day or two later) but the damage is usually quickly resolved. Tompkins believes the muscle repair processes to clean up that damage may be broken in ME / CFS – hence the often day or two delay before peak PEM symptoms hit. Given the central role the mitochondria play in the muscle repair process, he believes they may be involved as well.
The GistThe ME / CFS StudiesOne study will extensively examine the molecular components of the blood to try and understand why the hearts of one subset of ME / CFS patients are not receiving normal amounts of blood (preload failure). That same study will try to understand why the blood returning to the heart of another subset has higher than normal oxygen content. The higher than normal oxygen content indicates that the oxygen the muscles need to extract from the blood in order to exercise is not getting extracted. Another international study will do intensive analyses of muscle biopsies from ME / CFS patients at rest in an attempt to begin to understand why exercise is so difficult. The working hypothesis is that inflammation produced during exercise is damaging the muscle fibers and impacting the muscle repair process. |
In an attempt to uncover mitobiogenetic (mitochondria-biologic-genetic) biomarkers in the muscles, UK researchers will biopsy ME / CFS patients’ muscles, and send them over to Harvard, which will then dive into their “omics” (genomic, proteomic, phospho-proteomics, gene expression (high throughput RNASeq) and metabolomics ((glucose, lactate, ATP, etc.). They’ll also examine the muscle structure in fine detail. Lastly, they’ll send some muscle samples to Sweden to test for the presence of the metabolic trap.
What they won’t be able to do in the first study – but would really like to – is include an exercise stressor. It turns out that Mass General, the first site in the U.S. to employ an Institutional Review Board (IRB), takes its mission seriously. It takes it articularly seriously when muscle biopsies are concerned, making an already demanding review process even more “complicated and prolonged”. Mass General won’t allow them to do an exercise study first, so the first study will examine the muscles at rest, which will pave the way for a before and after exercise study.
Cashing In: The ICPET Omics Study
Next, the group will “cash in” on a fantastic resource – David Systrom’s blood samples gathered from people with ME / CFS doing invasive cardiopulmonary exercise tests (ICEPT’s). Systrom, a pulmonologist at Brigham and Women’s Hospital on the Harvard campus, has gathered a massive collection of oxygen-rich arterial and oxygen-depleted venous blood samples.
(Oxygen-rich blood flows through the arteries to the muscles where the oxygen gets used up and the depleted blood is moved to the veins which return it to right-hand side of the heart. The right-hand side of the heart then moves it to the lungs, where it gets oxygenated, and flows to the left-hand side of the heart, where it gets pumped back into the arteries…)
Systrom’s found two forms of “preload failure” in ME / CFS – a low-flow and a high-flow group.
Low Flow (Normal Oxygen)
In the low-flow group, sympathetic nervous system problems may be causing some venous blood to get shunted to the arteries, thus reducing the amount of blood that returns to the heart (preload failure).
Importantly, the oxygen content of this group’s venous blood is normal – meaning that the muscles are taking up normal amounts of oxygen from the arterial blood. The muscles, however, appear to be getting low levels of blood, thus putting them at risk for hypoxia, lactate and CO accumulations.
High-Flow (Low Oxygen)
The high-flow group has a entirely different problem. Their blood flows are normal, but the oxygen content of their venous blood is not.
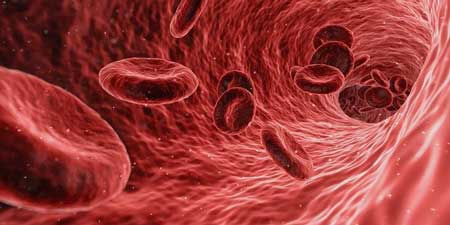
In their case sufficient amounts of blood appear to be getting to the muscles, but the muscle cells are not pulling normal amounts of oxygen from it. Either the capillary blood is getting pulled away into the microcirculation before it reaches the muscles, or the muscle cells themselves are having trouble utilizing the oxygen in the blood.
The Harvard Collaboration is going to examine the cytokines, proteomics and metabolomics in both groups. Their study is in the IRB approval process now. Tompkins is confident the study will uncover important new findings about ME / CFS.
These new technologies are illuminating, but what they aren’t is cheap. An in-depth examination of Systrom’s samples will cost between $1,000-$1,500 per sample. The three time points (before, during and after exercise) means 90 samples need to be analyzed for a 30-person study.
Tompkins is well aware of the NIH’s intransigence regarding ME / CFS. All this work, he said, should be funded on the NIH’s dime but it’s not. Everything that’s happening at the Harvard Collaboration is being funded by patients contributing to the Open Medicine Foundation. Tompkins and Xiao will use the data they gather for grant applications, but for now it’s the patients and their supporters that are keeping this work alive.
Conclusion
The interest Tompkins has received from both doctors and researchers is gratifying, and is probably in no small part to what one could call the “the Ron Davis effect” – an effect which occurs when a major researcher takes on ME / CFS. Things basically just start to move.
The same has clearly happened with Tompkins who seems to been able to elicit a significantly greater degree of interest in ME / CFS from medical specialists at Harvard than elsewhere. Those specialists are meeting regularly with Tompkins to streamline and improve their approach to ME / CFS.
Tompkins major (major) goal is building a Center of Excellence for ME / CFS and related diseases on the Harvard campus. It’s a huge undertaking but in some ways the hardest part is done: the interest is there and Tompkins believes he could quickly staff one right now.
Lastly, the Harvard ME / CFS collaboration has two studies underway. One, an international collaboration involving the U.S., the U.K. and Sweden, will probe more deeply into the muscles of people with ME / CFS than has ever been before.
The other will extensively analyse David Systrom’s blood samples in an attempt to understand what’s happening with the two subsets Systrom’s invasive exercise tests have uncovered in ME / CFS. One is characterized by low blood flows with normal oxygen levels, while the other is characterized by normal blood flows which reach the heart with higher than normal oxygen levels – indicating that the muscles have not received the fuel (oxygen) they should have.
Ron Tompkins With Llewellyn King


Shared with permission by Cort Johnson. To see the original article, please visit HealthRising.


